Last year, during Black History Month, we reflected on the impact the coronavirus pandemic had had on older Black people in the UK. For Black History Month 2021 we look again at the data and some of Age UK’s own research, to see what has changed, what more we know now, and what that tells us about the presence of health inequalities.
Looking back at where we've come from
Revisit our article on the impact of COVID-19 on older Black people from last year, part of our series of Black History Month content.
Black History Month 2020
Read the introduction to last year's Black History Month content, as well as articles on inspirational figures, the Windrush scandal, and community and culture
Increased risk
Black older people have experienced higher mortality from COVID-19 throughout the pandemic than White older people. This difference was particularly stark during the first wave of the epidemic, through the spring and summer of 2020, when coronavirus infections were more heavily concentrated in the larger towns and cities of the UK where most of the UK's Black population live. However, even in the second wave – when infections became more widespread across the UK – Black older people were more likely to die from COVID-19 than White older people. Research from the Office for National Statistics shows that in the second wave Black African men were more than twice as likely to have died from coronavirus than White British men, and men and women from all Black ethnicities were at increased risk compared to White British men and women.
Unexplained differences
Since the beginning of the pandemic we have heard about the increased risk that people who have pre-existing conditions are at when it comes to coronavirus. Some have wondered whether the higher death rates among Black people are due to higher rates of certain pre-existing conditions. Research from Public Health England looked into this and found it was not the case: Black people with some common pre-existing conditions, including cardiovascular disease and hypertension, were twice as likely to have died of coronavirus than white people with the same condition. Part of this difference was because Black people had been more likely to catch coronavirus, but part of the difference went unexplained: given the same age, sex, pre-existing conditions and many other characteristics, Black people were both more likely to catch coronavirus and more likely to have died of it if they caught it.
We're now well out of the devastating second wave of coronavirus that hit the UK last winter. However, coronavirus is still circulating in our communities and hospitalisations, and deaths continue. Do the ethnic inequalities we saw in previous waves of the pandemic persist? More recent research, by the Intensive Care National Audit and Research Centre, found that a higher than expected percentage of people currently in hospital with coronavirus are Black – they estimate that we would expect around 1 in 20 people critically ill with coronavirus to be Black, but the current figure is substantially higher, at more like 1 in 11.
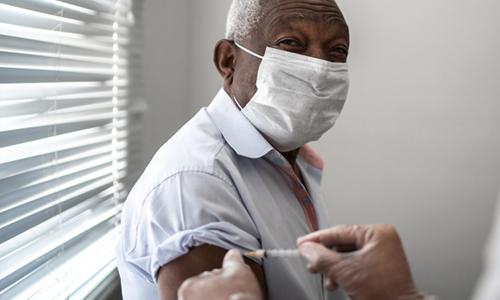
The difference vaccinations have made
The major difference between the situation now and during the first two waves of coronavirus is that many of us have been vaccinated, giving substantial protection against infection, hospitalisation and death from coronavirus. However, vaccinations can be another source of ethnic inequality. The Office for National Statistics looked at which older people had received coronavirus vaccinations in the UK up to the middle of April this year. Among older people aged 50+ they found that 67% of Black Caribbean and 71% of Black African older people had had at least their first coronavirus vaccination, compared to 94% of White British older people.
Recognising the inequalities
Explanations for these inequalities usually rest on an understanding that members of the UK's Black communities are more likely to feel hesitant about vaccination than people of some other ethnicities. Research by Age UK and other organisations has highlighted that some Black people have concerns about the coronavirus vaccines because they do not trust the Government, are concerned about the safety of the vaccines because of how quickly they were developed, and because they see a lack of ethnic diversity among the people taking part in the trials for the vaccines.
It is therefore vital that the Government, the NHS and other information providers ensure that they're going to sufficient lengths to communicate with people who are hesitant about vaccination on their own terms, to ensure that the UK's Black communities can feel confident in the safety and efficacy of the vaccines. Then, we may see that ethnic inequalities in vaccine uptake are reduced to a minimum and Black communities can receive the protection against coronavirus that other communities now have. And as well as vaccine hesitancy, it is important to consider whether there are inequalities in access to vaccination, and to take measures to remove any barriers to access.
As we look to a post-pandemic future, it's important to consider how the pandemic has affected all of us and our communities. Those communities – including the UK's Black communities – which have lost the most through deaths to coronavirus are also often those which have lost in other ways. In the year prior to the pandemic, Government data showed that 3 in 10 of the UK’s Black pensioners were in poverty. Age UK is soon to publish research with older ethnic minority people in England which shows that a fifth feel worse off financially since the pandemic began, and more than a quarter of older ethnic minority people have increased feelings of loneliness.
These challenges require our attention and action.
Breaking down the barriers of ethnic inequalities in health
One of the reasons that ethnic inequalities in health arise is because of the barriers older ethnic minority people experience in accessing health and care services. What are these barriers and why do people of colour face them?