Dr Elizabeth Webb, Senior Research Manager at Age UK, has an MSc in Epidemiology from the London School of Hygiene and Tropical Medicine and a PhD in Social Epidemiology from University College London. Here she examines why the evidence on coronavirus has led to the Government's special guidelines for those aged 70 and older.
On 16 March, Prime Minister Boris Johnson announced new measures to try to slow the spread of COVID-19, or coronavirus, in the UK. Although this guidance was directed at everyone, he emphasised that it is particularly important that people aged 70+, as well as younger people with particular medical conditions and pregnant women, practice social distancing.
This guidance seems very strict, and some have complained that it is ageist of the Government to address this guidance to all aged 70 and over, regardless of how good their health is. So, how did the Government come to their decision to give this advice?
The evidence
The main piece of scientific evidence comes from a report written by group of researchers, who form Imperial College London’s COVID-19 Response Team. They have taken learnings from the COVID-19 epidemics in China and Italy and have applied these to the situation the UK currently faces.
As COVID-19 is a very new disease, the science on how it works is still emerging, so there are lots of things that we aren’t certain of. However, the team at Imperial have looked at the data from China and Italy and seen:
- After people are exposed to with COVID-19 it takes between 1 and 14 days for symptoms to show, but the average period of time is 5 days. Epidemiologists call this period the incubation period.
- Before people show symptoms of COVID-19 they are contagious – that is, they are able to pass on the virus to other people – for a period of time, which the Imperial team think is about 12 hours. People then continue to be contagious while they have symptoms.
- The average person with COVID-19 passes the virus onto 2.4 other people, if they aren’t isolated from other people. This is what epidemiologists call the reproduction number.
The reproduction number is crucial
It is the reproduction number that is crucial in determining how quickly an epidemic spreads. If every person with the virus gives it to a further 2 people, we can easily go from 1 case, to 2, to 4, to 8, and so on. In order to slow the growth of an epidemic we need to reduce the reproduction number.
If we are able to reduce it to 1 or below, where the average person with the disease passes it on to less than 1 other person, then the epidemic stops growing. This is what the Imperial team referred to as suppression of the epidemic, and others have referred to flattening the curve, in order to avoid overloading the NHS.
Containment measures
In order to suppress an epidemic we can use containment measures. Many have been discussed over the past few weeks, with some now recommended by the Government. The job for the team at Imperial College was to work out how much the reproduction number would be reduced by each of the containment measures, in order to get it below one and suppress the epidemic. We have all, therefore, been asked to practice social distancing.
Differing severity for different people
However, the evidence from China and Italy let the Imperial team know that not everyone who gets COVID-19 is affected the same way. Some people experience very mild symptoms, and some people, sadly, die.
The team used the information we have from the epidemics in China and Italy to work out who was most at risk of needing to be in hospital or of dying, in order to best reduce the number of people this happened to.
We’ve all heard that COVID-19 is harder on older people. Despite many areas of uncertainty around COVID-19 and how and why it affects people as it does, the evidence for this is stark.
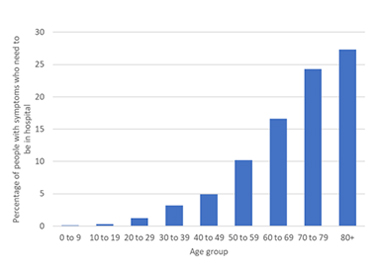
Risk of hospitalisation increases with age
In this graph below we can see how the risk of needing to be admitted to hospital increases steadily with age. For people under the age of 50 the risk is less than 5%, or 1 in 20. For people aged 70 and over the risk is greater than 20%. Around one in four people aged 70 and over who have symptoms of COVID-19 will need to be admitted to hospital.
Age UK's coronavirus information hub
Information on coronavirus, including updates on how you can look after yourself and loved ones, comments from Age UK, and ways you can support older people.
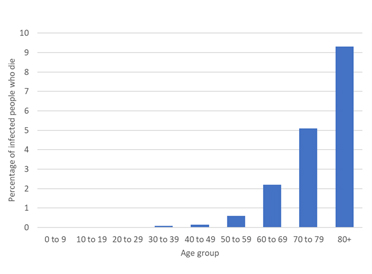
A more serious statistic
As well as people being more likely to be hospitalised with COVID-19 if they are older, this second graph shows how the risk of dying from COVID-19 increases with age. At younger ages, there is very low risk of dying, but there is a steep and steady increase in the chances for those aged 50 and over. For people in their 70s, the risk of dying from COVID-19 is just over 5% – 1 in 20 – and at ages 80 and over this risk is just over 9%, or 1 in 11.
Evidence leads to advice
It is this information that has led to government advice suggesting those aged 70 and over take the advice to practice social distancing even more seriously than others. They have assessed the risks and determined that, for people aged 70 and over, the risk of being hospitalised and of dying of COVID-19 are too high, both for the individual themselves, and for the NHS to cope with if too many people of these ages catch COVID-19.
More information is needed
As the science on COVID-19 is so new, we don’t know exactly why older people are at greater risk. This isn’t always the case: with flu, we see very young and very old people at higher risk alike, and during the last really big flu epidemic, in 1918, it was young adults who were at the greatest risk.
However, although we don’t yet understand COVID-19 completely, what we see from the COVID-19 pandemic across the world tells us very clearly that those aged 70 and over are at increased risk if they catch COVID-19. Because of this, Age UK wants to encourage and support people aged 70 and over to follow the guidance, and practice social distancing.
 No one should be left behind
No one should be left behind
As lockdown lifts, you can help us make sure vulnerable older people aren't forgotten. Donate today to help Age UK open doors for our older generation.
Source: Ferguson, N et al, 2020. ‘Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand.’ Accessed here.

More pieces by Dr Webb
Dr Elizabeth Webb is a Senior Research Manager at Age UK. She has an MSc in Epidemiology from the London School of Hygiene and Tropical Medicine and a PhD in Social Epidemiology from University College London.
- What's the science behind the Government's guidelines?
- Can we predict how coronavirus will progress?
- Why are older people more at risk from coronavirus?
- How can we recognise when we have coronavirus?
- How close are we to a vaccine?
- How can you assess your own risk from coronavirus?
- What is k and who are the super-spreaders?
- Is there an increased risk of coronavirus for BAME older people?

